Neuraxial anesthesia is a widely used technique for providing pain relief during surgeries and labor, but its application after spine surgery presents distinct challenges. Anatomical changes caused by surgeries such as laminectomies, spinal fusions, and disc surgeries complicate the ability of anesthesiologists to locate critical spaces for needle insertion. Scar tissue, hardware implants, and modifications to vertebral structures can obscure landmarks typically relied upon for epidural or spinal anesthesia. While there are some best practices anesthesiologists can follow to mitigate these challenges, further innovations are needed to improve safety and efficacy in this area. Here’s what we know.
Spinal hardware and its impact on neuraxial anesthesia
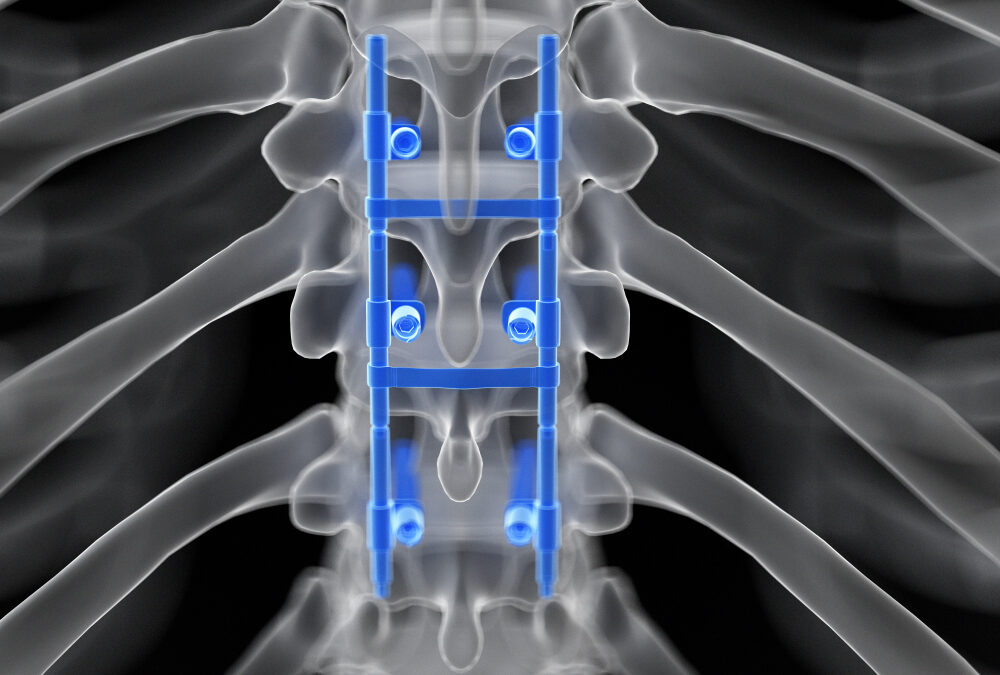
In patients with a history of spine surgery, the presence of implants — such as rods, screws, plates, or cages designed to stabilize the spine — significantly alters anatomy.
- Hardware placements: Metal rods and screws are frequently placed along the vertebral column to stabilize it.
- Spinal fusions: Spinal fusion procedures create continuous segments of bone, eliminating the intervertebral spaces.
- Scar tissue: Healing from surgery often results in scar tissue, which might form with high variance in location and density.
These anatomical alterations may increase risks like inadvertent dural puncture or an inability to pass small gauge spinal needles. And they underscore the need for tools that allow anesthesiologists to navigate altered anatomy with greater accuracy and safety.

Challenges of neuraxial anesthesia after spine surgery
Spinal hardware presents unique difficulties when performing neuraxial anesthesia. Accessing essential spaces such as the epidural and subarachnoid regions is often more challenging due to a range of factors:
- Obscured landmarks: Metal rods, plates, and screws disrupt the traditional anatomical landmarks that anesthesiologists use to determine needle insertion points. When these landmarks are altered or blocked, the spinous process and lamina become unreliable indicators.
- Scar tissue formation: Dense scar tissue from prior surgeries can block the path of the needle, necessitating multiple attempts that not only increase patient discomfort but also raise the risk of complications.
- Unknown anatomy: While surgical reports may offer some insights, they often lack the level of detail anesthesiologists need to fully understand the altered anatomy. Vertebral modifications or segment removals may obscure key areas, making it difficult to predict the exact location for anesthesia administration.
- Hardware placement interference: Implants, particularly metal ones, can influence or obstruct the needle path due to anatomical alterations, making traditional approaches impossible in certain cases. When the needle encounters hardware, anesthesiologists are forced to redirect or change insertion levels, increasing the risk of trauma or incorrect needle placement.
Best practices for neuraxial anesthesia after spine surgery
Despite the challenges posed by altered anatomy and spinal hardware, several best practices are proving valuable for clinicians seeking to improve outcomes for patients with these modifications:
- Preoperative imaging: Advanced imaging techniques such as MRI or CT scans can provide crucial anatomical insights before the procedure, allowing anesthesiologists to strategize and prepare accordingly. However, CT imaging is generally avoided in pregnant patients due to radiation exposure. For pregnant patients, imaging information would typically need to be obtained pre-pregnancy or from historical records.
- Consultation with surgical team: Working closely with the surgical team provides anesthesiologists with a clearer understanding of how the spine was altered and helps them determine the safest approach. Use imaging findings and procedural flexibility to address potential barriers. Real-time adaptations are often still necessary due to the unpredictability of scar tissue density and location.
- Alternate needle approaches: In cases where traditional midline approaches are obstructed, a paramedian approach — one of several techniques that might be considered — can allow anesthesiologists to bypass midline scar tissue or hardware for safer needle insertion. As always, approach selection should consider individual patient anatomy and imaging findings.
Ultrasound may also be invaluable for pre-procedural planning, allowing anesthesiologists to identify available spaces for needle placement and navigate challenging anatomies with higher accuracy and lower patient discomfort.

What solutions are still needed?
While advancements in imaging and technique have improved the ability of anesthesiologists to perform neuraxial anesthesia on post-spine surgery patients, ongoing improvements are still more than worth pursuing. And it starts with pointed conversations among anesthesia providers and medical innovators.
Current imaging tools, such as ultrasound and MRI, provide valuable pre-procedural insights by visualizing scar tissue and hardware. However, advancements that improve real-time guidance during needle advancement — beyond static pre-procedural imaging — could greatly enhance precision and safety in complex cases. Standardization or technological optimization of real-time imaging solutions would allow anesthesiologists to dynamically navigate altered anatomy, actively avoiding scar tissue and hardware during needle insertion.
While several established guidelines exist for neuraxial anesthesia in patients with altered anatomy, further research is needed to refine approaches that consider individual variations while aligning with standardized protocols. The development of universally accepted, evidence-based guidelines could help anesthesiologists approach these cases with greater consistency, reducing variability and improving patient outcomes. The development of education programs and simulation training specifically designed to address the challenges of altered spinal anatomy might also better prepare anesthesiologists for difficult cases, supporting both patient safety and clinical efficiency.
Elevating precision in neuraxial anesthesia after spine surgery
At RIVANNA, we believe in equipping clinicians with the best tools and knowledge to overcome challenges in neuraxial anesthesia after spinal surgery, particularly when it comes to cases involving altered anatomy. By addressing these challenges head-on and sharing best practices, we can collectively improve patient safety and outcomes. We encourage anesthesiologists and healthcare providers to continue this dialogue, sharing experiences and strategies for managing these complex cases.