Neuraxial anesthesia is a critical procedure that can be challenging for clinicians and anxiety-inducing for some patients. The traditional reliance on blind palpation for needle placement presents significant challenges, particularly in complex procedures such as epidurals, where the margin for error is exceedingly narrow. As a result, patients may experience unnecessary discomfort, and clinicians are often faced with the challenge of balancing precision with efficiency.
At RIVANNA, we are committed to transforming the healthcare landscape and addressing the challenges that patients and clinicians face. Over the past decade, our focus has been on developing imaging-based medical technologies that improve procedural outcomes and enhance the human experience. I have always believed that precision is a form of compassion — and with innovations like Accuro Neuraxial Guidance, we have taken that belief and turned it into a tool that empowers anesthesiologists to deliver safer, more efficient, and ultimately more compassionate care.
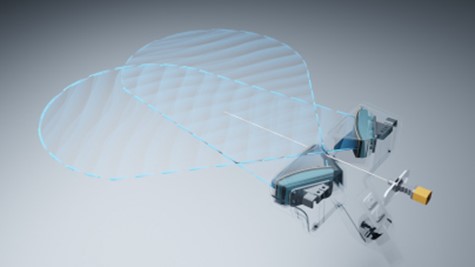
This journey began with Accuro as a handheld device. Now, we are pushing boundaries again with Accuro 3S — a system that will bring enhanced real-time needle visualization to neuraxial anesthesia. This innovation is a direct response to what anesthesiologists have been asking for, and it is the next frontier in ultrasound-guided regional anesthesia.
Current limitations of ultrasound in neuraxial anesthesia
Traditional neuraxial anesthesia techniques have long relied on blind palpation, where clinicians use touch to locate anatomical landmarks such as the spinous processes and interspinous spaces. While this method is widely used, it is far from perfect, especially when patients have challenging anatomical features, such as obesity, scoliosis, or poorly defined landmarks. In these cases, needle misplacement is not uncommon, leading to failed blocks, multiple needle insertions, and patient discomfort.
Although ultrasound has shown promise and is gradually being explored for neuraxial anesthesia, its use in practice is still limited in scope. While some experienced anesthesiologists use ultrasound dynamically, many clinicians still use it primarily as a pre-procedural tool, like a stud finder for the spine, scanning the patient’s anatomy and marking key points on the back before introducing the needle.
This method offers valuable assistance, though there are opportunities for improvement: patient movement or displacement of skin markings can make it difficult to rely on pre-imaging during needle advancement. Importantly, there is no real-time feedback to help the clinician visualize the needle as it moves through tissue toward the epidural or subarachnoid space.
Clinical studies have shown that residents using ultrasound for pre-procedural marking observe an improvement (with stronger trends observed in obese patients) over traditional blind techniques — reducing the need for needle redirects. Experienced anesthesiologists have also achieved improved first-insertion success rates guided by pre-procedural ultrasound. But it does not fully address the challenges of real-time needle guidance. Once the imaging is complete, the clinician lacks continuous feedback during needle advancement, which is when precision is most critical.

The innovation behind Accuro 3S
The development of Accuro 3S is rooted in the needs of anesthesiologists who consistently expressed a desire for real-time needle visualization to mirror the way ultrasound is used in other regional anesthesia procedures. The technical challenges to achieving real-time needle visualization in neuraxial procedures were substantial:
- Unlike peripheral nerve blocks, which permit lateral access with the needle, neuraxial procedures necessitate midline access — the needle must pass directly in line with the ultrasound probe. This requires a specialized probe that allows for simultaneous imaging of the spinal anatomy and needle without obstruction.
- Clinicians performing epidurals or spinal blocks encounter what is known as the “three-hands problem” — needing to hold the ultrasound probe in one hand, the needle in the other, while simultaneously managing the syringe to monitor loss of resistance.
The Accuro 3S will introduce an innovative approach to neuraxial ultrasound. Equipped with AI-enabled software and a unique probe design, it will provide clinicians with continuous, in-plane needle tracking. The addition of a novel patient drape will effectively address the “three-hands” problem by enhancing probe stability. These advancements, along with automated identification of key anatomical landmarks, position Accuro 3S to streamline complex spinal and epidural procedures, offering practical solutions to long-standing challenges in neuraxial anesthesia.
This new system is poised to transform the way neuraxial anesthesia is performed. Accuro 3S may allow clinicians a more adaptive and reliable way to guide the insertion of a needle via more sophisticated and fool-proof viewing planes, improved versatility, and more ergonomic needle control.
The future of neuraxial anesthesia and RIVANNA’s vision
As we look toward the future of neuraxial anesthesia, it is clear that real-time procedural guidance is just the beginning. While Accuro 3S addresses one of the most pressing challenges in neuraxial anesthesia — precise real-time needle tracking — there are still other areas ripe for innovation. For instance, improving the accuracy of loss-of-resistance techniques, potentially through automated pressure sensors or robotics, could further reduce human error and make these procedures even safer.
We also see vast potential for applying this technology into chronic pain management. In the United States alone, approximately one quarter of the population present with severe and incapacitating chronic pain annually, and many rely on spinal injections for chronic pain management. These procedures often employ fluoroscopy for image guidance.
Although fluoroscopy is effective, it involves ionizing radiation, which carries risks for both patients and clinicians. With the development of Accuro 3S and other ultrasound-based solutions, there is an opportunity to bring safer, non-radiation-based alternatives to chronic pain management, particularly in countries where fluoroscopy is not as widely reimbursed.
At RIVANNA, we are also continually exploring new ways to leverage our AI and ultrasound imaging technologies to solve the challenges clinicians face, all while improving patient safety. For example, we are currently developing our Accuro XV musculoskeletal imaging platform for automated bedside fracture assessments with ultrasound. In efforts like these, we remain committed to pushing the boundaries of medical innovation in service of resolving historically unmet clinical needs — globally.

Join us in expanding compassionate, technology-driven care.
As RIVANNA’s co-founder, chairman, and CEO, my mission — which is always a collective mission for our teams and partners — is to elevate standards of care to improve decision-making, health outcomes, and patient safety. I believe the best way to do that is by solving the real, everyday challenges clinicians face. We are reimagining the way procedures are performed to reduce patient discomfort and improve clinician confidence. Every challenge we have encountered has driven us to innovate. And with every solution we discover, we aim to contribute to advancements that are essential in modern medical practice.
Ultimately, it is not just about the technology. It is about the millions of patients and providers who will benefit from safer, more efficient medical interventions. We are giving clinicians the tools they need to take control of outcomes. And knowing that we are on the cusp of several breakthroughs that could change the face of anesthesiology and emergency medicine for good, I am proud of the work we have done. More than that, I am excited for what is next.
